This page is for you if:
The information on this page can help you to learn more about the genetic testing that is available to you to identify if you have also inherited the same BRCA2 gene fault.
If you have any questions, or would like to discuss proceeding with genetic testing, please contact us at:
- Your family member has informed you that they have had genetic testing through BRCA-DIRECT, and
- We identified an inherited BRCA2 gene fault.
The information on this page can help you to learn more about the genetic testing that is available to you to identify if you have also inherited the same BRCA2 gene fault.
If you have any questions, or would like to discuss proceeding with genetic testing, please contact us at:
Overview
Why is this genetic test being offered to me?
We all have genes whose job is to help keep us healthy. Some genes help to protect us against developing cancer. Sometimes, faults in these ‘cancer protection’ genes contribute to an increased risk of developing certain types of cancer.
We have identified one of these gene faults (sometimes called “pathogenic variants,” “gene alterations” or “mutations”) in one copy of your relative’s BRCA2 gene.
We have identified one of these gene faults (sometimes called “pathogenic variants,” “gene alterations” or “mutations”) in one copy of your relative’s BRCA2 gene.
What is the chance I have a BRCA2 gene fault?
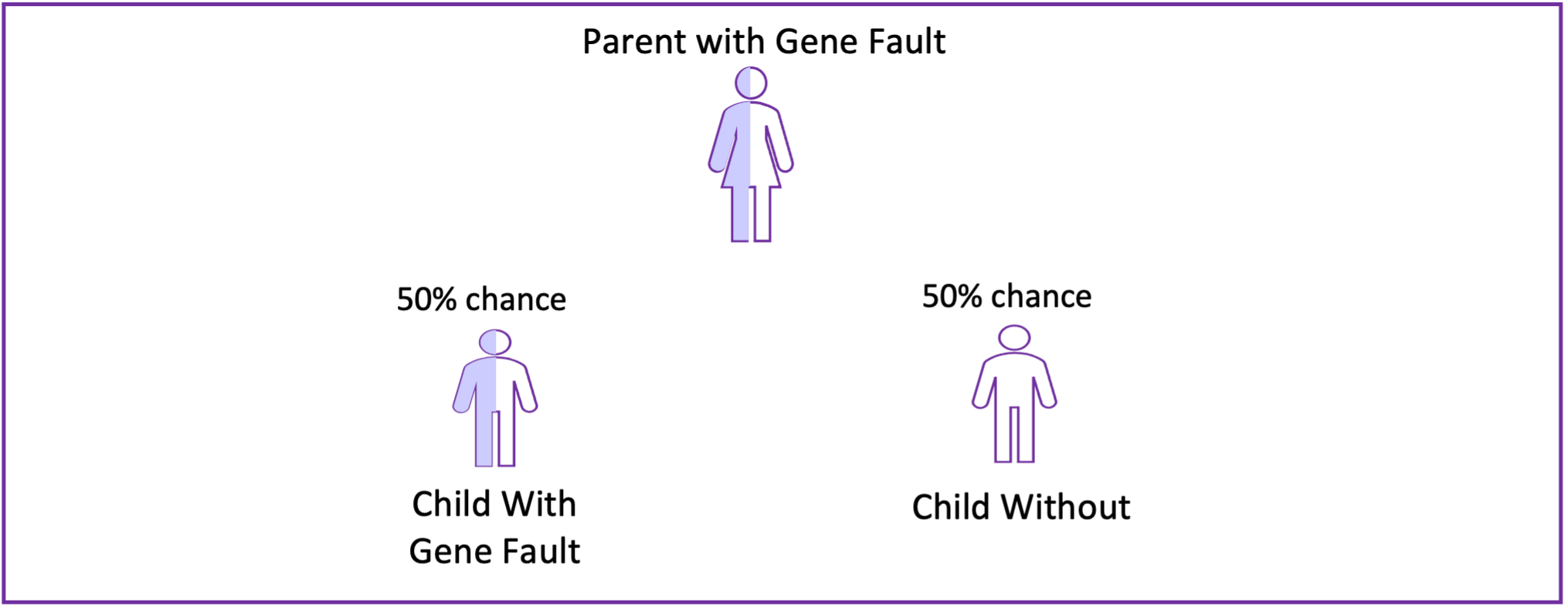
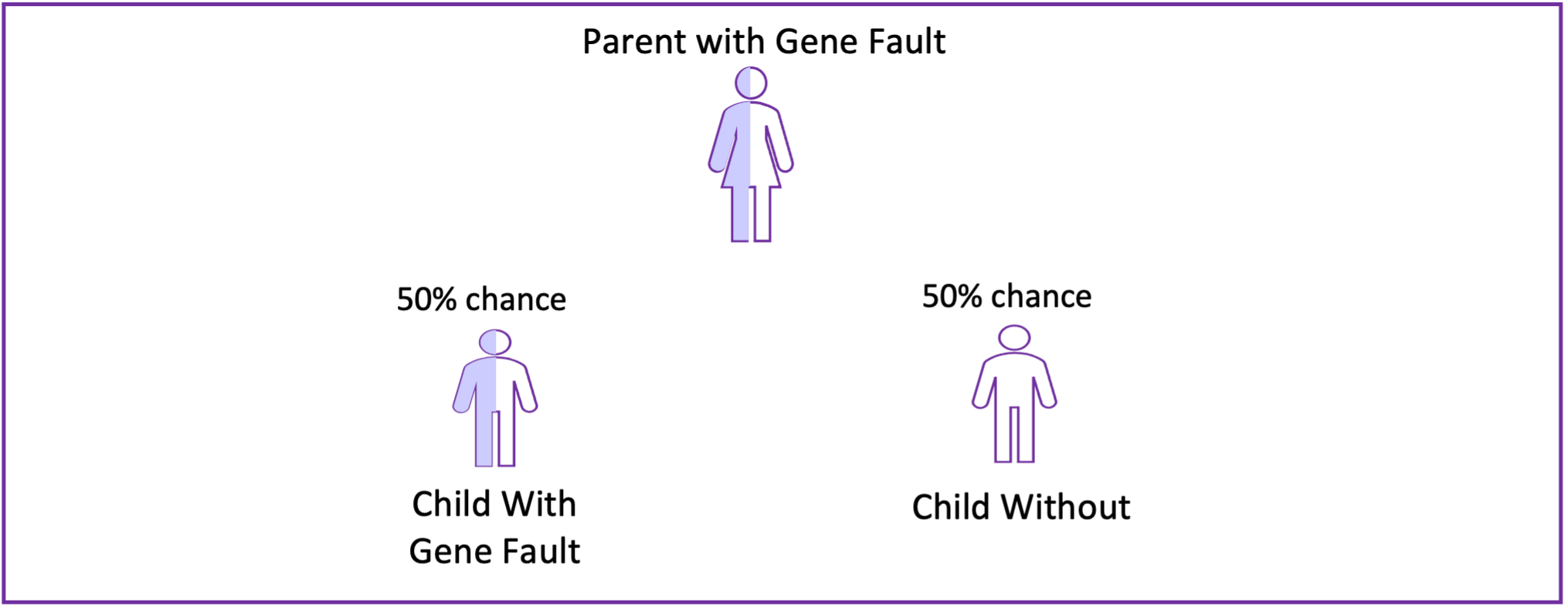
- The chance that you have inherited the same BRCA2 gene fault depends on how closely related you are to this relative. If you are a first degree relative (for example, parent, sibling, child), there is a 50% chance (1 in 2) that you have the same gene fault
- There are associated cancer risks with these gene faults for both men and women, so it is beneficial for everyone to consider genetic testing
- Both men and women can have, and pass down, BRCA2 gene faults. Every time a person with a BRCA2 gene fault conceives, there is a 50% chance (1 in 2) that the child inherits the gene fault
Why is this genetic test helpful?
- This genetic test can identify if you have inherited the BRCA2 gene fault in your family
- BRCA2 gene faults increase the risk for certain types of cancer. Learning if you have a BRCA2 gene fault can:
- open cancer risk management options for you
- open cancer risk management options for your relatives
- provide information for family-planning
Cancer Risks
If you have a BRCA2 gene fault, it does not mean that you will definitely get cancer, but it does mean you have a higher chance for certain cancers.
- The main cancers caused by BRCA2 gene faults are female breast cancer and ovarian cancer.
- The tables below show the detailed cancer risks for females and males. Ranges are given, as the risk to each individual depends on multiple factors including family history.
| Female Cancer Risk Over Lifetime (to age 80) | ||
|---|---|---|
| Cancer | General population | With BRCA2 gene fault |
| Breast | 11.5% | 69% (61-77%) |
| Ovarian | 1.5% | 17% (11-25%) |
| Pancreatic | 1.0% | 2% (1-4%) |
| Male Cancer Risk Over Lifetime (to age 80) | ||
|---|---|---|
| Cancer | General population | With BRCA2 gene fault |
| Breast | Less than 0.1% | 4% (2-8%) |
| Prostate | 12.5% | 27% (21-35%) |
| Pancreatic | 1.0% | 4-5% (approximate) |
BRCA2 gene faults are not associated with childhood cancers, except in very rare cases where a child inherits a fault in the same gene from each parent.
Sources: Cancerresearchuk.org; UKCGG BRCA2 Germline Pathogenic Variant Carriers Management Guidelines for Healthcare Professionals
Managing Cancer Risks
Learning if you have an BRCA2 gene fault can allow you to proactively manage your cancer risk. If you are found to have a gene fault, you will be able to discuss the management options below and more with your clinicians. They can provide more individualised information to support you in making the decisions best for you.
- Female Breast Cancer Risk Breast screening is the main option for managing breast cancer risk for women with a BRCA2 gene fault:
- Ovarian Cancer Risk There is currently no proven effective screening for ovarian cancer. Therefore, women with BRCA2 gene faults are offered surgery to remove the ovaries and fallopian tubes. This makes the risk of developing ovarian cancer much lower. This surgery is called a risk-reducing salpingo-oophorectomy. The surgery is typically performed after a woman has completed their family, and not before the age of 40.
- Male Breast Cancer Risk We advise men to become familiar with the look and feel of their chest wall, to know what is normal for them. If they notice any changes to their normal chest feel or appearance, they should report them to their GP.
Results
If you decide to proceed with genetic testing, your results will be ready approximately 6 to 12 weeks after you provide your saliva sample (see steps to proceed below)
There are two possible outcomes of this genetic test: you have inherited the gene fault (positive result) or you have not inherited the gene fault (negative result)
- We will send your genetic test result by post, along with a copy of your genetic test report. We will also copy the letter and test report to your GP.
- Your result letter will have a front sheet so that you may choose when to read your result
- Our genetic counsellors are available to speak with you whilst reading your result, If you would like their support, please call the genetics helpline (020 3437 6514)
There are two possible outcomes of this genetic test: you have inherited the gene fault (positive result) or you have not inherited the gene fault (negative result)
1) You have inherited the BRCA2 fault (a "positive" result)
What does this result mean for me?
- This result indicates that you have a higher risk for breast and ovarian cancer (females) or breast and prostate cancer (males).
- We will schedule a follow-up telephone appointment with a genetic counsellor for within a week of you receiving your result, to talk about this test result in detail, and provide an opportunity to ask questions. If you prefer, you may telephone the genetics helpline and speak to a genetic counsellor sooner, and at a time of your choosing.
- We will refer you to your local clinical genetics service for further consultation and ongoing management.
2) You have not inherited the BRCA2 fault (a "negative" result)
What does this result mean for me?
- This result means that no increased risk of breast and ovarian cancer was identified. Your cancer risk is likely the same as other people your age.
- You should still participate in routine cancer screening offered to all people through the NHS (for example, mammograms for women over 50) and report any symptoms to your GP.
- If you have a strong personal or family history of cancer, you should report this history to your GP. They may refer you to clinical genetics for consideration of further consultation and additional genetic testing.
Additional Services
Who might benefit from different/additional genetic testing services?
- If you are unsure about testing and/or would like to have a more detailed consultation, you may contact your GP to be referred to your local clinical genetics service
- If you have already had cancer, you are still eligible to participate in this programme. However, you may also be eligible for additional genetic testing, and you may wish to discuss this with your GP.
Implications for Relatives
- If you have a BRCA2 gene fault, your adult relatives who are eligible for NHS care can access NHS genetic testing. Their GP will be able to refer them to their local clinical genetics service. We can also provide letters to share with your relatives to help them access this service.
- Sharing of genetic information in your family can be done in discussion with you or through a process that will not personally identify you.
Family Planning
- Some individuals or couples choose to have genetic testing before family planning. There may be additional reproductive options (for example, pre-implantation genetic testing) available to couples if one or both partners have a BRCA2 gene fault. These options help couples to avoid passing on the gene fault to their children.
Management of Data and Samples
- To understand and classify gene alterations, we need to compare information about the genetic alterations we have found nationally across the NHS and internationally (without sharing any patients’ names). Sometimes, with new information, we will reclassify a gene alteration. We may recontact you in the future if new information about the classification of your gene alteration becomes available.
- Normal NHS laboratory practice is to store DNA samples, as they may be used for future analysis (for example if additional gene tests are required) and/or to ensure that other testing (for example that of family members) is accurate and of high quality.
Genetic Testing and Insurance
Genetic testing and insurance
The insurance industry differentiates between a predictive genetic test and a diagnostic genetic test
- If you have not had a cancer, the BRCA2 genetic test is termed a predictive test . Insurance companies cannot ask you to disclose the results of predictive genetic tests for the majority of policies.
- If you have had a relevant cancer, the BRCA2 genetic test is termed a diagnostic test. Insurance companies may ask you for the results of your genetic test if you open a new life, income protection or critical illness insurance policy. Any policies already in place will not be affected.
-
You can find more information about insurance from the Association of British Insurers:
www.abi.org.uk/data-and-resources/tools-and-resources/genetics/genetic-testing/ - Royal Marsden NHS Foundation Trust, Beginners Guide to BRCA1 and BRCA2: https://patientinfolibrary.royalmarsden.nhs.uk/brca1brac2
Additional information and support
Genetic counsellors are available to discuss any of this information in more detail. They are here to support you with any individual concerns or questions. To speak with a genetic counsellor, please call the genetics helpline.
 Alternatively, you may contact us by email at [email protected]
Alternatively, you may contact us by email at [email protected]
Below are some links for further information and support. These are generic resources, and some information may not be relevant to you.
Steps to proceed
How to proceed with the genetic test and provide your saliva sample
Please watch this video that explains what steps you need to take to proceed with your genetic test and provide your saliva sample. Alternatively, follow the steps below.
This content is shared from YouTube by Google. Whilst we have taken steps to enhance your privacy, by viewing this video you are accepting that your information may be shared with Google, including tracking of your internet activity through use of cookies. You can find more information about how Google uses your information by viewing their privacy notice (please note this links to an external website).
- Consent Form
- Read and sign the Genetic Test Consent Form.
- Please note that we cannot process your sample if your Genetic Test Consent Form is incomplete
- Personal Details Form
- Fill in the requested information
- Saliva Sample
- Wait at least 30 minutes after eating or drinking before sample collection
- Wash your hands thoroughly
- Rinse your mouth well with water to clear away any food
- Fill the tube with your saliva up to the line
- Screw on the lid and check it is tight
- Wash your hands again thoroughly
- Write the date of saliva collection on the adhesive label, then stick the label on the saliva collection tube
- Place the labelled saliva collection tube into the Speci-Pouch following the instructions on the label
- Post from a Post Office
- Place both forms and the packaged saliva sample in the pre-paid plastic mailing bag
- Take the package to your local post office. You may find your nearest post office at: www.postoffice.co.uk/branch-finder
- This package may NOT be posted using a street post box
If you have any questions or would like to discuss further, please contact our genetics helpline at
020 3437 6514
or email [email protected]