Information for breast cancer patients
This page is for you if:
- You have recently been diagnosed with breast cancer.
- You are thinking about having genetic testing in relation to your breast cancer.
- Your clinical team has provided you with a BRCA-DIRECT testing pack.
How will this information help you?
This information has been designed to help you:
- Learn more about the genetic testing offered through BRCA-DIRECT
- Understand what genetic testing means for you and your family.
- Complete your genetic testing pack at home.
Please watch our short information video:
- To watch the video in Indian Punjabi, Pakistani Punjabi, Urdu and Bengali, click here
Additional resources for you:
- A digital copy of the information booklet is available to download via this link. This booklet has also been translated into Indian Punjabi, Pakistani Punjabi, Urdu and Bengali.
- Click this link to jump to our video guide to support you with collecting a saliva sample at home.
- Click this link to navigate to our document library where you can access all of our resources.
Why might I have this genetic test?
A sample of your saliva is sent to the laboratory where DNA is removed from the cells. We read the DNA of these genes to see if there is a change to the DNA sequence that disrupts how the gene works. This is known as a gene fault.
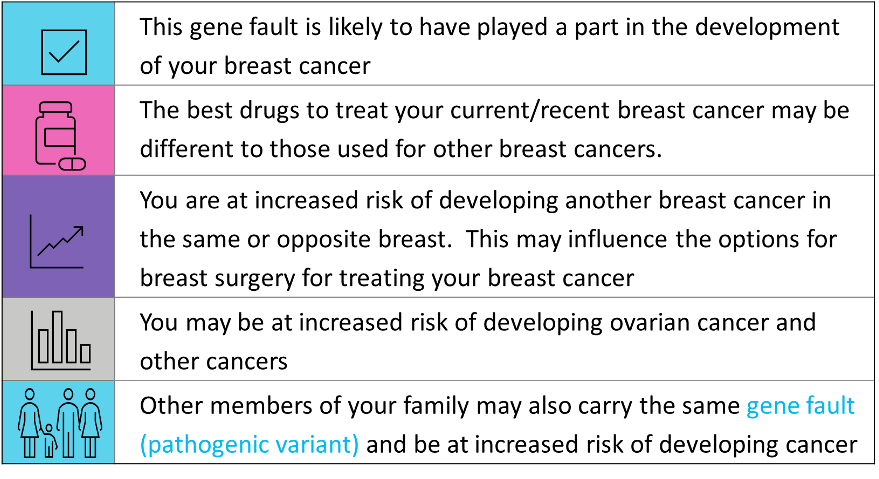
The results of the genetic test may give useful information to you and your clinicians about:
- Why you developed breast cancer and the best treatment options available for your breast cancer.
- Whether or not you are at higher risk of developing a new breast cancer in the future.
- Whether or not you are at high risk of developing other cancers, such as ovarian cancer.
- Whether or not your family members (both male and female) are at increased risk of developing breast and other cancers associated with these genes.

Why might I choose not to have this test now?
You may choose not to have a test at this time. Genetic testing is a personal choice. If you're unsure about genetic testing, our Genetic Counsellors are available to discuss your options with you. You can contact them via our helpline: 020 3437 6514.
There may be reasons why you may prefer not to have a genetic test at this time.
- It can be emotionally difficult for some people to learn that they have a gene fault. Some people find this information overwhelming alongside their breast cancer diagnosis and treatment.
- Some people are concerned about the implications of a genetic test on their health insurance policy. We cover more about genetic testing and insurance here.
- If you already know that there is a gene fault in your family, you may wish to be referred by your GP directly to clinical genetics for testing and support.
If you are interested in genetic testing, but would like to defer to a later date.
BRCA-DIRECT is a time-limited program being offered in some hospitals to any woman with a new diagnosis of breast cancer. You may or may not be eligible for NHS genetic testing in the future.
- You can have the genetic test through our programme.
- We anticipate the programme will close in July 2024, but it may close earlier.
- You may need to supply a new saliva/blood sample and consent form.
- If you are eligible, you can have an NHS test at any time in the future. Your GP, or sometimes your oncologist, can refer you to your local clinical genetics services.
- Fewer than 1 in 5 (20%) women with breast cancer are eligible for standard NHS genetic testing.
-
Some women choose to pay for a genetic test from the private sector. We advise discussion with a trusted knowledgeable healthcare professional if you are considering this option as some private providers may offer unreliable tests and information.
If you are interested in genetic testing, but would like to defer to a later date, you may speak to your clinician or call our genetics helpline to learn more about your options.
What can the test tell me about my breast cancer?
This genetic test helps find out if your breast cancer was caused by a gene fault. This information can help you and your clinicians make choices about treatments and/or breast surgery.
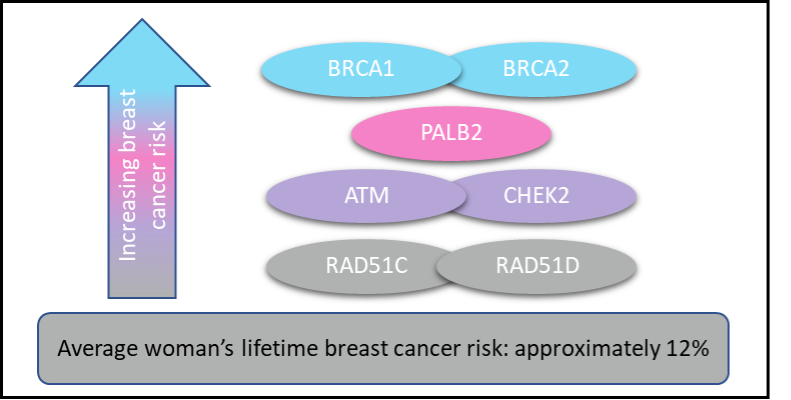
The average woman has a 12% risk of developing breast cancer in her lifetime. Meaning approximately 12 out of 100 women may develop a breast cancer in their lifetime. A gene fault can increase a woman’s breast cancer risk further.
Faults in the seven genes tested are associated with differing levels of increase in breast cancer risk.
- Faults in BRCA1/BRCA2 genes are associated with a higher lifetime risk of breast cancer of approximately 70%. Meaning approximately 7 in 10 women with a BRCA1/BRCA2 gene fault will develop breast cancer.
- Faults in the other genes (eg ATM or CHEK2), also increase the breast cancer risk, but less than BRCA1/BRCA2.
- Breast cancer risk will also be influenced by other factors in addition to the gene fault, such as family history of cancer, personal diet, smoking, lifestyle and other risk factors.
What can the test tell me about my risk of new cancers in the future?
There are different cancer risks associated with each of the seven genes on this test. If the genetic test finds that you have a gene fault, you will have appointments in Clinical Genetics and be given detailed information about your risks and management options related to that gene.
There are different cancer risks associated with each of the seven genes on this test.- The increased risk for developing a new breast cancer in the future varies gene-by-gene.
-
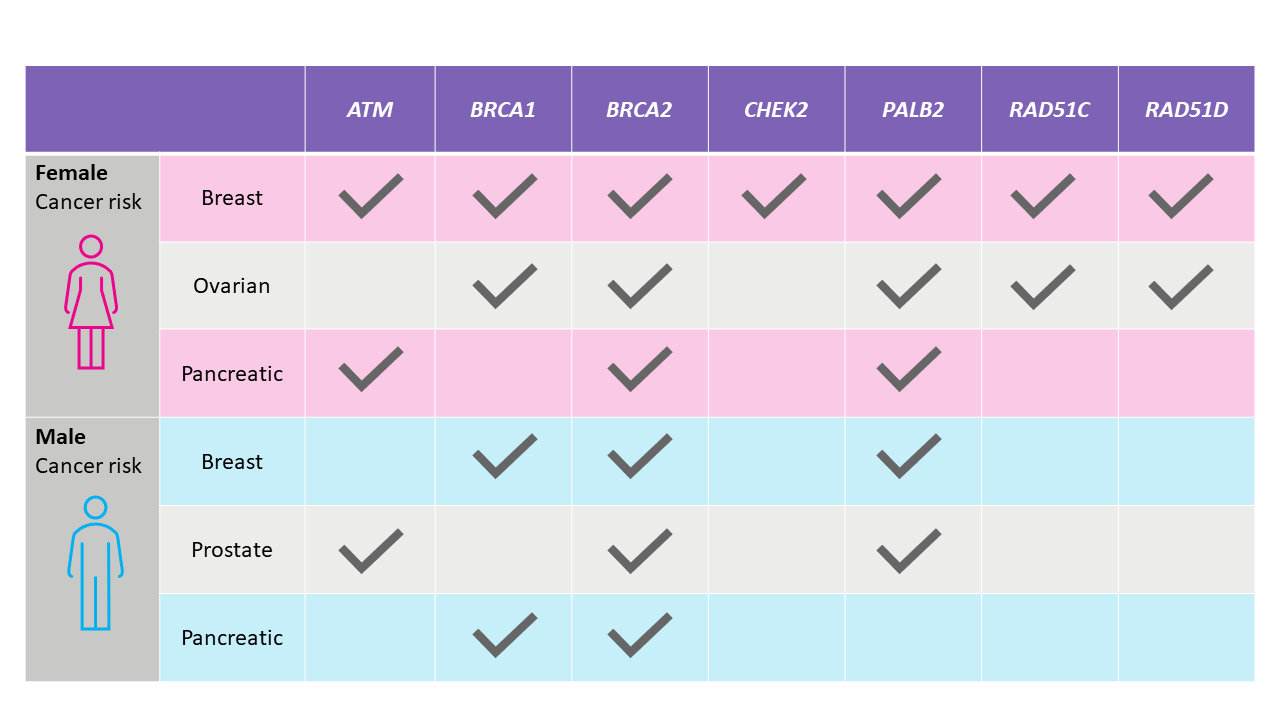
Some of the genes are also associated with an increased risk of certain other types of cancer in the future.
- For example, gene faults in BRCA1 and BRCA2 also increase the risk of ovarian cancer.
- The table below indicates where gene faults are known to increase risks of different types of cancer for each of the seven genes.
- The increased cancer risk varies for each of the cancer types and the genes.
Your individual risk of developing different cancers will also depend on your family history and personal factors (such as weight and alcohol intake).
We can provide more tailored advice to you about your future cancer risks if the genetic test finds a gene fault.
How can I manage my future cancer risk if I have a gene fault?
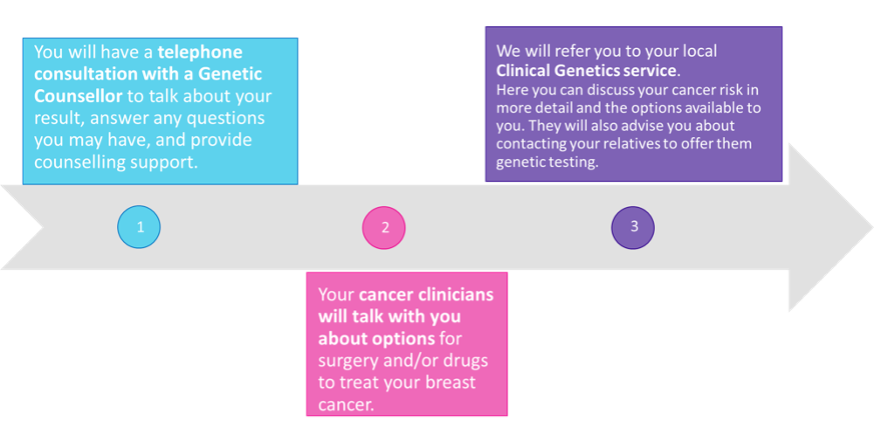
If the genetic test finds that you have a gene fault, you will have an appointment with a BRCA-DIRECT genetic counsellor, further follow-up appointments in Clinical Genetics, and be given detailed information about your risks and management options related to your specific gene fault.
Knowing that you have a gene fault can open more options for managing your risk.
- Cancer risk management options are different for each of the seven genes on this test.
- Options may include additional screening (for example, additional mammograms) or surgery (for example, removal of breast tissue or ovaries).
- If a gene fault is found, we will refer you to your local clinical genetics service for follow up care and long-term management. Your team will discuss your personal cancer risks and provide you with more detailed information about the options for managing your risk, supporting you with making decisions, and accessing appropriate services.
If you are interested in knowing more about the options, this is written below.
New Breast Cancer
-
Surgical prevention: For women with a high risk of developing another breast cancer, the risk of developing a new breast cancer can be reduced by having an operation to remove one or both healthy breasts. This is called risk-reducing mastectomy. Various types of breast reconstruction are available following risk-reducing mastectomy.
- Women with a new diagnosis of breast cancer and a gene fault may have the option to have both breasts removed (bilateral mastectomy) as part of their breast cancer surgical treatment, or more often at a later date.
- Female relatives without cancer who have also inherited the same gene fault may also be offered a risk-reducing mastectomy.
- Screening: Women with a gene fault may be able to access more regular screening for breast cancer through scans and/or mammograms with the intention of picking up any new breast cancers at an early stage. The ages between which women receive extra screening varies depending on individual risks, taking into account additional risk factors.
Ovarian Cancer
- Women over the age of 40 may be offered an operation to remove their ovaries and the fallopian tubes (tubes which carry eggs to the womb). This is often done as keyhole surgery, where the surgeon only needs to make a tiny cut to remove the ovaries and fallopian tubes.
Pancreatic Cancer
- Pancreatic screening is typically only offered as part of a research study, as there is no current NHS screening programme.
- Pancreatic screening involves scans or tests using an internal camera; it could be offered to certain people with a gene fault, especially if there is pancreatic cancer in the family.
Prostate Cancer
-
Research is still underway regarding the best way to screen for prostate cancer in men with gene faults and there is no current national NHS screening programme.
- Men with certain gene faults may be offered an annual blood test. Additional screening using blood tests, scans and removal of samples (biopsies) from the prostate may be offered as part of a research study.
What do the results mean for my family?
Gene faults are inherited. Meaning if you have a gene fault, other people in your family may also have the same gene fault. Your family members would be able to access genetic testing and options for managing their risk if they are also found to have the gene fault.
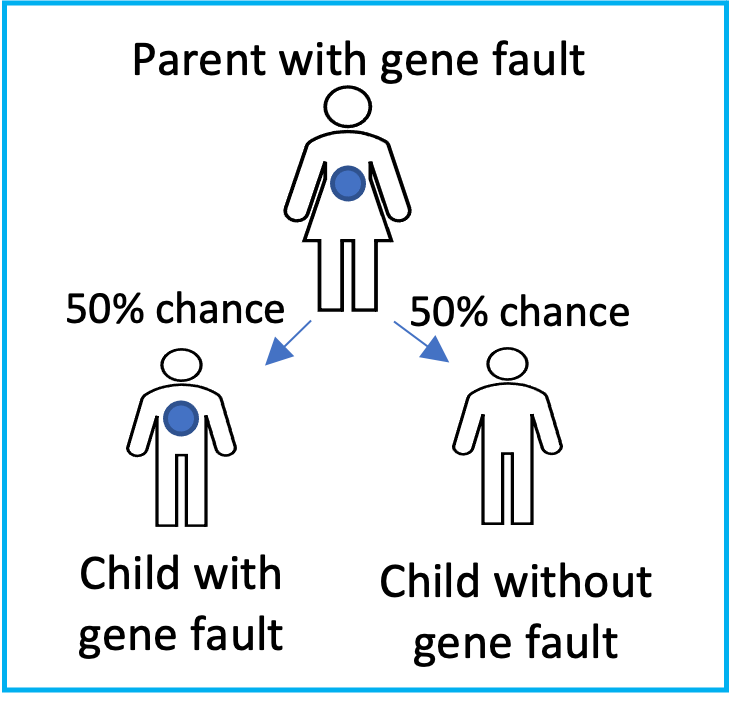
Both men and women can have and pass down gene faults.
We all have 2 copies of every gene (one we inherit from our mother and one we inherit from our father). Each parent only provides one set of their genes to each child. So if you have a gene fault in one of these genes, you could have inherited it from one of your parents. This also means other people in your family may have the same gene fault.
-
Children: If you carry a gene fault each time you have a child, there is a 50% chance (1 in 2) you will pass on the gene fault to the child and a 50% chance (1 in 2) that you will not.
- If you do not have children and are considering starting a family, there may be family planning options available to prevent passing on the gene fault, if you feel this is important to you.
-
Your other first-degree relatives (siblings and parents) also have a 50% chance (1 in 2) of having the same gene alteration.
Adult first-degree relatives can access a genetic test to see if they have the same gene fault (a process sometimes called cascade testing). Sharing of genetic information in your family can be done in discussion with you or through a process that will not personally identify you.
They can access this testing in two ways:
- Contact our programme directly by contacting our helpline and speaking with one of our genetic counsellors. This option may only be available for a time-limited period whilst the BRCA-DIRECT programme is running.
- Ask their GP for a referral to their local clinical genetics service.
-
Your second-degree relatives (aunts, uncles, grandparents) have a 25% chance of having the same gene fault.
Typically, second degree relatives will only be offered this test after the first degree relative you both share has had a chance to consider if they want to have the genetic test (and been shown to have the same gene fault). In some instances, for example if that shared relative is no longer with us, they may still be able to access the genetic test, in the same two ways above.
If any of your relatives would like to talk about the possibility of genetic testing, and learn more about what it might mean for them, they can call our genetics helpline on: 020 3437 6514.
Genetic testing and insurance
The insurance industry differentiates between a diagnostic genetic test and a predictive genetic test. You can read about the difference between these below.
This genetic test which you have been offered is termed a diagnostic test because you have previously been diagnosed with breast cancer.
A diagnostic test is when you have a genetic test following diagnosis of a condition.
For example, this genetic test following your diagnosis of breast cancer.
A predictive test is when you have a genetic test for a condition that runs in your family, but you currently have no signs or symptoms of that condition.
For example, if you have a gene fault, and then your family member chooses to have genetic testing, their test is considered a predictive test providing they have not had a relevant cancer.
You can read more about the agreement between the British Government and the Association of British Insurers on this website:
https://www.abi.org.uk/data-and-resources/tools-and-resources/genetics/code-on-genetic-testing-and-insurance/
Results
If you would like to have support from a genetic counsellor while opening your results, please telephone the genetics helpline (+44 20 3437 6514).
There are three possible test results:
Around 5 out of 100 (5%) women with breast cancer will receive a positive result from this genetic test, meaning a gene fault has been found.
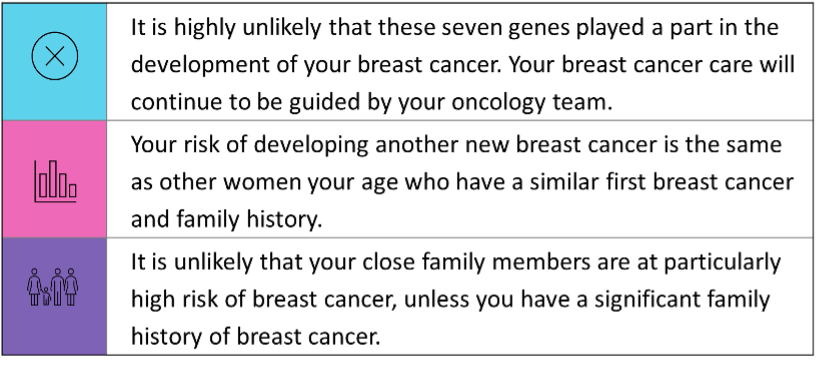
Approximately 93 out of 100 (93%) women with breast cancer will receive a negative result from this genetic test. This means that we did not find any harmful gene faults.
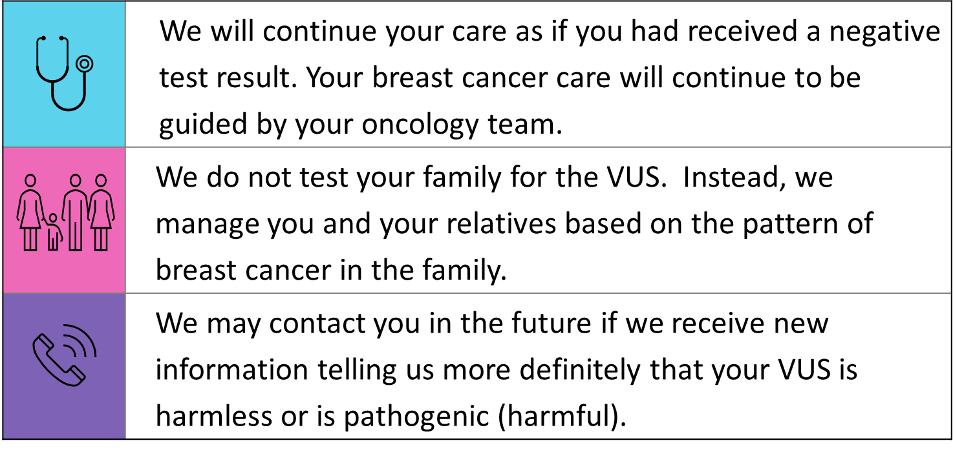
Around 2 out of 100 of these genetic tests (2%) will return a VUS result.
A VUS is a type of gene change that we are unable to clearly interpret as either harmful or not harmful.
Management of data and samples
The genetic testing will be completed by the Centre for Molecular Pathology at the Royal Marsden NHS Foundation Trust, part of the North Thames Genomic Laboratory Hub.
What information will be held about me?
We will retain securely within your electronic health record all information relating to your genetic testing, including your referral, genetic test consent and results.
How will your data be used?
To understand and classify gene changes, we need to compare information about the gene change we have found nationally across the NHS and internationally. If we need to do this, we do it securely, and without sharing any identifiable information such as your name.
Will I be contacted in the future if new information arises?
Sometimes, with new information, we will reclassify a gene change. You may be recontacted in the future if new information about the classification of your gene change becomes available.
What will happen with my saliva sample?
We will store your DNA sample according to normal NHS laboratory practice, which currently requires us to store your sample for at least 30 years.
Your DNA sample may be used for future analysis (for example if additional gene tests are required) and/or to ensure that other testing (for example that of family members) is accurate and of high quality.
Where can I find more information?
More information about how the Royal Marsden processes and stores information is available on their website: https://www.royalmarsden.nhs.uk/privacy.
Additional information and support
 Alternatively, you may contact us by email at [email protected]
Alternatively, you may contact us by email at [email protected]
Below are some links for further information and support. These are generic resources, and some information may not be relevant to you.
- Breast Cancer Now: breastcancernow.org
- Macmillan: www.macmillan.org.uk
- Prevent Breast Cancer: preventbreastcancer.org.uk
- Royal Marsden NHS Foundation Trust, Beginners Guide to BRCA1 and BRCA2: patientinfolibrary.royalmarsden.nhs.uk/brca1brac2
Steps to proceed
How to proceed with the genetic test and provide your saliva sample
- Consent Form
- Read and sign the Genetic Test Consent Form.
- Please note that we cannot process your sample if your Genetic Test Consent Form is incomplete
- Personal Details Form
- Fill in the requested information
- Saliva Sample
- Wait at least 30 minutes after eating or drinking before sample collection
- Wash your hands thoroughly
- Rinse your mouth well with water to clear away any food
- Fill the tube with your saliva up to the line
- Screw on the lid and check it is tight
- Wash your hands again thoroughly
- Write the date of saliva collection on the adhesive label, then stick the label on the saliva collection tube
- Place the labelled saliva collection tube into the Speci-Pouch following the instructions on the label
- Post from a Post Office
- Place both forms and the packaged saliva sample in the pre-paid plastic mailing bag
- Take the package to your local post office. You may find your nearest post office at: www.postoffice.co.uk/branch-finder
- This package may NOT be posted using a street post box